Wallowa Memorial capacity severely tested during most recent surge
Published 2:15 pm Monday, August 30, 2021
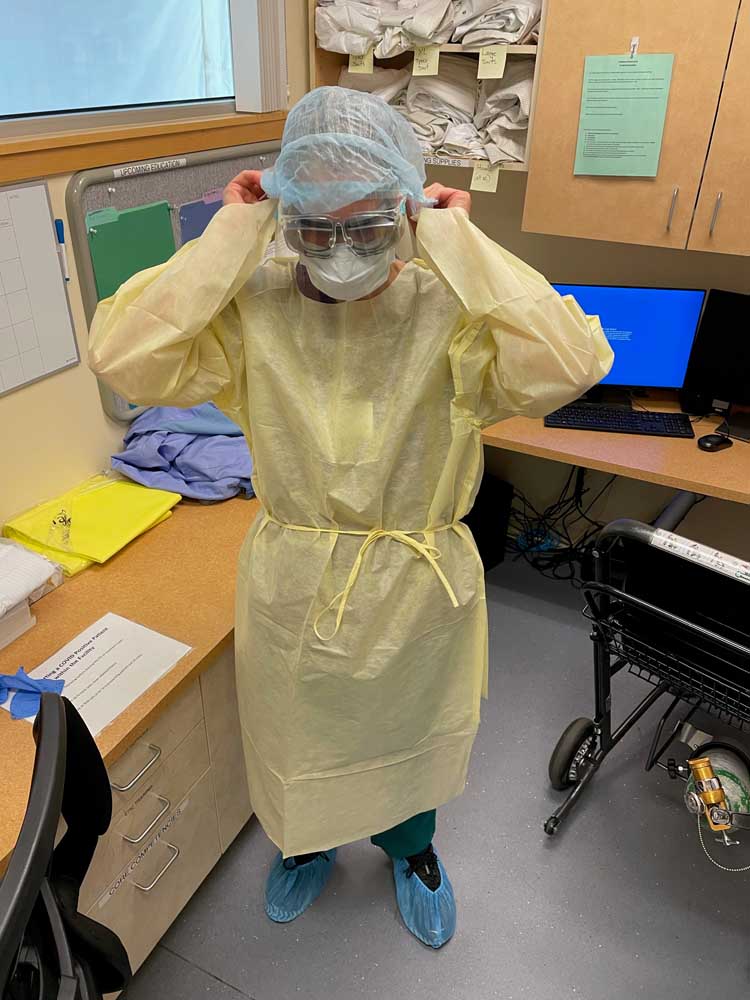
- Wallowa Memorial Hospital nurse Karla Holmes, R.N., prepares to see a patient diagnosed with coronavirus. Cases have been rising sharply in Wallowa County and WMH on several occasions in the past month has reached its capacity.
ENTERPRISE — Statewide, hospitals have been near or even at their capacity, with more than 1,100 people in Oregon hospitalized due to coronavirus and the state exceeding 90% capacity.
Wallowa Memorial Hospital has been in a similar situation.
Brooke Pace, WMH communications director, said during the past month, the hospital has reached its patient capacity several times.
She clarified, though, that that doesn’t necessarily mean all 25 beds at WMH are full. The staffing availability also has to be taken into account.
“We have reached capacity a number of times since the beginning of August,” she said. “That doesn’t mean we’ve had 25 patients. It means we’ve gotten to the point that we’re taking care of as many patients as we physically can.”
Stacey Karvoski, the hospital’s quality director, said the acuity of the patients — how much care they need — also is a consideration.
“Hypothetically, we could have seven patients in the hospital and that is all we can take care of if the acuity is high,” she said.
Pace said WMH has been asked if they have the ability to take on extra patients, but has had to turn those requesting hospitals down.
“We have not had the ability to accept them,” she said.
Pace said the hospital is working with Wallowa County Emergency Management to request additional personnel from the National Guard, anticipating a need for extra help in nursing, emergency medical services, and more.
Significant increase
While the exact number of coronavirus patients to enter WMH in the past month wasn’t available, Pace said several have been through the hospital doors.
“We can certainly say there has been a significant increase in coronavirus patients at our hospital,” she said.
Given the critical-access nature of the hospital, Pace said WMH does not have an ICU, and, thus, no patients in ICU care in the hospital. Like with any situation, a coronavirus patient requiring ICU care would be transferred to a different hospital.
Patients have been transferred from WMH in the past month, though the specific reasons were not given.
Statewide trends seen locally
Reports throughout Oregon have shown that more young people are among those being hospitalized with coronavirus.
Karvoski said that is consistent with what WMH is seeing.
“These patients are younger …” Karvoski said.
“…And (have) a higher level and severity of respiratory issues,” Pace added. “… It would be safe to say that Wallowa County’s trend has matched that of the state.”
That also includes, she added, the ratio of hospitalized patients who are vaccinated or not vaccinated against coronavirus. Statewide, OHA data shows that through the first two weeks of August, just less than 3,000 of the more than 20,000 coronavirus cases reported were breakthrough cases, meaning more than 85% of coronavirus cases in those two weeks were in unvaccinated individuals.
Karvoski said at this point, though, nurses at WMH have not had to take on a higher patient count than they typically would.
“Right now, I think we’re able to stick with our staffing plan and our patient load for the nurses has remained pretty much the same,” she said.
Pace said, too, that staff is under a lot of pressure and stress with the ramped up number of patients, but that it remains committed to serving the community.
“It’s unfortunate we are being placed in this situation” she said. “Staff are stressed and tired with the case load. It’s been a long road.”
Contingency plan
What happens if the hospital did get overrun with patients? Or it cannot transfer patients?
While that hasn’t happened, Pace said there is a roadmap for the hospital in case there was a surge.
“It has not reached that level yet, but that is certainly part of our surge plan is preparation for if things continue to get worse,” she said.
The contingency plan, she said, is detailed with action plans depending on the types of patients in the hospital. If, for example, there were a surge in coronavirus patients, the physical therapy wing and medical office building that houses Wallowa Memorial and Winding Waters medical clinics would be converted into a “clean space” to house patients hospitalized but who don’t have coronavirus.
“We can increase the number of beds in our medical surge floor for COVID patients,” Pace said.
Karvoski added that there could be an additional 21 beds added, if necessary.
Vaccine mandates
With the FDA’s approval of the Pfizer vaccine on Monday, Aug. 23, the clock is officially ticking toward Gov. Brown’s vaccine mandate deadline that all medical staff are to be fully vaccinated — which means two weeks past their final shot of a vaccine — by Oct. 18. That means the first doses of a vaccine would have to be administered on Sept. 6 (Moderna vaccine), Sept. 13 (Pfizer) or Oct. 4 (Johnson & Johnson).
The OHA has granted the option for individuals to submit a religious or medical exemption as opposed to receiving a vaccine.
Pace said given the recent FDA approval of the Pfizer vaccine, and that there is still “grey area” WMH is seeking to clarify with the exemptions, it’s unclear how the mandate will affect WMH and its staff.
Getting a boost(er)
Booster shots of the Pfizer or Moderna vaccine will be made available starting Sept. 20, Pace said.
The CDC and FDA have recommended that immunocompromised individuals should receive an additional dose of the mRNA vaccines — Pfizer or Moderna — they originally received.
Pace said, though, the booster shot shouldn’t be received until eight months after a person received their second shot. Those eligible Sept. 20 would be those who received their second dose on Jan. 20.
A booster has not yet been recommended for those with the Johnson & Johnson vaccine, Pace said.








