At home genetic tests of limited use
Published 11:56 pm Monday, November 13, 2017
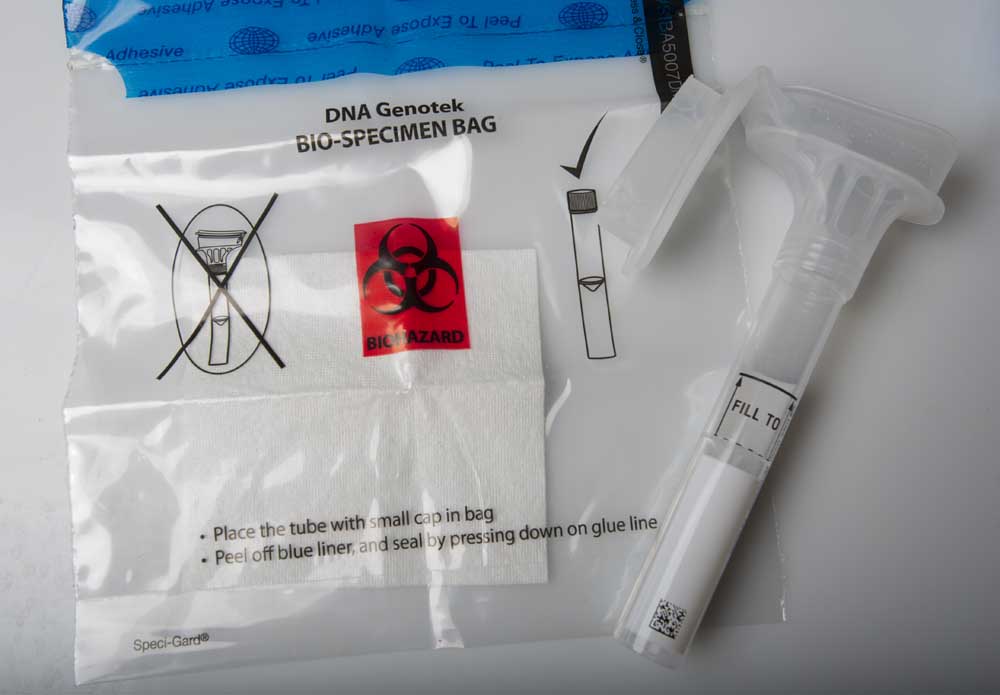
- At left, a genetic testing kit mailed by 23andMe. Named for the 23 pairs of chromosomes normally found in human cells, 23andMe was founded just over a decade ago and received a multimillion-dollar financial boost from Google.(Ryan Brennecke)
The advent of at-home genetic testing offers people a tantalizing power: the ability to look at their genes and see what conditions or diseases they are likely to develop. Like the introduction of X-rays or CT scans that allowed doctors to see inside bodies without cutting them open, genetic testing offers a glimpse at a person’s future, and perhaps, a chance to change it.
But like the early days of imaging, the view provided by early-stage genetic testing can be just as grainy or clouded. The still-developing nature of the direct-to-consumer genetic testing industry has sparked a fierce debate among genetics experts and the medical community about the value and the dangers of such tests. While some maintain such genetic tests can empower individuals to take steps to counter their genetic risks, others believe the tests are more misleading than helpful.
“I usually say it’s mostly for entertainment,” said Barb Pettersen, a genetic counselor in Bend. “And you can’t make major health decisions based on that information.”
Spit in a tube
Direct-to-consumer genetic tests, such as those marketed by Mountain View, California-based 23andMe, require consumers to send in a biological sample, generally some saliva. Customers can order a test kit online, spit in the tube and mail it back. Within two months, they get a report detailing their genetic risk for 10 conditions, including things like Alzheimer’s disease or Parkinson’s, blood clots or celiac disease.
Although the company goes to great lengths to help individuals understand what those results actually mean, most consumers are likely overestimating their significance. That’s because the company isn’t analyzing all of a person’s genes nor reporting on all of the genetic factors that have been linked to various diseases.
Instead, the company is looking for about a half-million single nucleotide polymorphisms, known as SNPs. An SNP is a variation of the genetic code that occurs in at least 1 percent of the population. Researchers have been able to show that certain variants increase the risk for a given condition, while others may lower it.
Geneticists caution that while SNPs represent the most common genetic variants, they aren’t necessarily the most useful. A given SNP may be present in a lot of people, but only increase a person’s risk for a disease a small amount, what geneticists call low-penetrance. High penetrance variants, on the other hand, increase a person’s risk for a disease substantially, but are often much more rare.
Moreover, 23andMe is allowed by the FDA to report on only 10 health conditions, giving only a small slice of a person’s genetic health risks.
“The SNPs that they do report have high analytic validity, meaning they have done their homework in making sure that what they report out is actually present in your genome,” Pettersen said. “But it may not have clinical validity, meaning there may not be enough studies showing, yes, this actually is a marker that increases your risk for Parkinson’s, for example, or they may not have adequate data to say, yes, the relative risk for Parkinson’s is three times the population rate.”
SNPs generally account for a small increase in genetic risk, and genes work in concert with lifestyle and environment to cause disease. The tests rarely give a yes-or-no answer, leaving plenty of room for consumers to misinterpret their true risks.
Playing the odds
You can think of genetic risk like playing blackjack with a single deck of cards. The average risk for developing a condition could be 1 in 20, about the same odds of getting dealt two cards totaling 21, or a blackjack. If the first card is a 10 or a face card, however, your odds of getting a blackjack increase to about 1 in 13. And if you’re dealt an ace, the odds increase to 1 in 3. But as even casual gamblers can attest, getting a 10 or an ace is no guarantee of getting blackjack.
It’s the same with genetics. A given genetic variant can be like being dealt a 10 or an ace and can increase the odds of developing a condition a little or a lot, but it does not guarantee it.
To further complicate things, in blackjack, you could hit 21 by getting the right combination of three, four or five cards that add up to 21. Similarly, multiple genetic variants that individually don’t contribute much to the risk of developing a given condition, can increase risk significantly in combination with each other.
Genetic tests can also be confusing when results are presented in terms of the relative risk. A given variant could double or triple your risk for a disease, which sounds pretty scary. But if the average risk was 1 in 100,000, a doubling or tripling of that risk could still represent a rare occurrence.
Consumers also tend to put too much stock in genetic testing, compared with family history or lifestyle. Someone who is obese with a strong family history of diabetes might not have the genetic variant for Type 2 diabetes and so could discount his or her overall risk.
Several years ago, Bend resident Marcene Austin had been experiencing some digestive problems she suspected might be lactose intolerance. Her doctor suggested she try the 23andMe genetic testing to confirm it. When the test came back, however, she didn’t have the genetic variant that causes intolerance, but her results showed two variants with an increased risk for macular degeneration.
Years before, she had visited a school for the blind and underwent a simulation of how macular degeneration affects vision.
“I didn’t want any part of that,” said Austin, a retired IRS employee. “So when I got this back, I said I want to do everything I can, which includes taking the results when I go to the ophthalmologist in November.”
23andMe provided some guidance on what she could do about the risk. That includes not smoking — she doesn’t — and eating a healthy diet — she does.
“I’ll just continue with that with more of a focus on vegetables that are more colorful,” she said. “So for me, it’s an awareness that I want to do everything I can to stave off something I don’t want.”
Austin, 70, and her husband, Dennis Lazzar, 73, had discussed whether they would want to know all of the information included in the test, including tests for Alzheimer’s and Parkinson’s.
“Do we want to know or do we want to hide our heads in the sand?” she said. “And we both agreed we want to know. I want to have a long, healthy life where I can live on my own independently as long as possible. And information is my friend, not my enemy.”
Understanding results
Researchers at the University of Michigan and Harvard/Brigham and Women’s Hospital have been tracking how consumers are interpreting their genetic test results. They’ve found for the most part consumers understand that the results can reveal an increased risk for developing a condition, not a certainty that it will happen. The Impact of Personal Genomics, or PGen, study found “neither excessive overreaction nor complete disregard” for the test results.
But they also found people tended to be skeptical of bad news but relieved by good news, and that good or bad news about Alzheimer’s tended to influence people the most.
“Although there are studies out there that say yeah, people generally get the gist of the results, I really haven’t seen that in my personal life,” Pettersen said. “Everybody definitely misinterprets it.”
One of the more common misinterpretations is believing that if the results don’t mention a high risk for a condition, that the person is safe.
For Parkinson’s, for example, 23andMe looks for one variant on each of two genes. But there are at least seven genes that have associations with Parkinson’s, and one each of the genes where the company is testing for one variant. There are hundreds of other variants that are not being tested.
“They are choosing the ones that are most common in a certain population. But if you’re negative for that, it really doesn’t change your overall risk for Parkinson’s by very much,” Pettersen says. “And I think that’s what people misinterpret is they don’t have these two variants, therefore (they think) their risk of Parkinson’s must be very low.”
Similarly, 23andMe reports on the Apolipoprotein E gene, commonly known as APOE, that has been linked with Alzheimer’s disease. Everyone has two copies of the gene, one from each parent, and they can have three versions, E2, E3 or E4. The E2 variant is the rarest, but carrying even one copy reduces a person’s risk of Alzheimer’s by 40 percent. Having one copy of E4 can increase your risk by two to three times, while two copies can increase the risk by 12 times. However, 23andMe only reports on the presence of E4.
But someone who has the E2 and E4 gene variants would have a much lower risk than someone with E3 and E4. And someone who has two E3 gene variants can still get Alzheimer’s, while another with two E4 gene variants could avoid it.
“The genes that they’re choosing to test puzzle us: Why these?” Pettersen said. “And we’re thinking, well, it’s because they got SNPs for these that work and they have information on them. If we were designing a clinical test that would be helpful to people for their own health and prevention, we would pick a whole different group of genes to study.”
23andMe officials denied multiple requests for an interview. In response to a question about how they chose their tests, they said, “We have a number of criteria that center on the value for our customers and the scientific validity behind any report we may offer.”
In fact, geneticists rarely make use of such broad-based genetic screening in patients, and generally don’t recommend screening for patients without a family history or some symptoms of a disease with genetic links.
Dr. Wojciech Wiszniewski, a geneticist at Oregon Health & Science University, says many of the patients he sees with medical problems have already had direct-to-consumer testing done, and bring those results to their appointment.
“It’s only kind of an indication that the patient is concerned and trying to get some answers,” he said. “But this is not something that helps me to establish diagnosis.
Instead, geneticists start with a family history and a medical history, then conduct a physical exam. If they suspect a genetic cause, they’ll recommend a specific genetic test to confirm it. Once confirmed they can use the medical diagnosis along with the genetic findings to optimize the treatment.
“It’s a different story, when somebody healthy is coming to the clinic,” he said.
Third-party sites
While 23andMe provides genetic risks for only 10 health conditions, it does allow people to download their raw data, including all of the other SNPs in the company’s tests. That’s spurred a cottage industry of third-party sites that will take that raw data and provide information on many more health conditions.
Some of those sites are run by academics and rely on peer-reviewed studies published in medical journals. Others are run as commercial ventures, with varying degrees of accuracy and validity.
But genetic experts warn that the raw data has not been fully validated by 23andMe, and the chances that data is incorrect are much higher than for the SNPs the company reports.
“The raw data is kind of in its own category,” said Brianne Kirkpatrick, a genetic counselor and founder of Watershed DNA. It hasn’t been confirmed to be error free and it hasn’t been repeated with different genetic technologies.”
Kirkpatrick has one client who sent her raw data to a third-party site. It told her she was a carrier of a rare recessive condition called Smith-Lemli-Opitz.
“Further research into it showed that it was a very common false positive finding with this particular company’s raw data and the analysis tool that was being used,” she said. “Because we read into the fine print a little bit further, we realized that this was most likely a false positive result for her.”
DNA testing is usually only done once in a lifetime because it stays the same. Once a profile is recorded, mistakes in raw data might never be corrected.
Some of the commercial sites do their own DNA processing, but many rely solely on uploaded raw data, and there’s no assurance they are using legitimate science in providing their results.
“Over time, we’ll probably achieve better information that will be useful to people,” Wiszniewski said. “But right now I think it’s pretty early in the game, and I think there are a lot of people making money off consumers.”
In 2006, the Government Accountability Office investigated a handful of websites offering to use genetic tests to provide personalized nutrition and lifestyle guidance. GAO found the sites mislead consumers by making unfounded predictions, often so ambiguous they have no meaningful use.
One site recommended personalized supplements — at a cost of $1,200 a year — that GAO found were no different from vitamins and antioxidants that could be purchased in any grocery store for $35 a year. Another site offered products that claimed to repair damaged DNA.
GAO had created nine different fictitious profiles all using the same DNA, but received vastly different recommendations from the four websites.
The Food and Drug Administration had blocked 23andMe from marketing its health tests in 2013, until the company provided more information on how they were reaching their findings and how they would help consumers understand their results. The FDA allowed them to resume genetic health testing earlier this year.
But so far the FDA has not intervened with most of the smaller sites. That’s allowed a lot of dubious genetic testing to continue. One site offers a “superhero” test that purports to tell you whether strength, intelligence or speed are your “superpower.” At least three sites offer DNA-based matchmaking services.
Pettersen recently identified at least 38 companies testing DNA for athletic ability, including some that will tell you what sport your child should play. One company has marketed an APOE E4 test as a way to determine if your child is at higher risk from concussions.
“I’m sure we’re going to have more and more companies and more and more tests offered this way. They’re trying to just place a foot in the door,” Wiszniewski said. “Somebody is going to try to stop it, so they need to make as many profits as possible.”
DNA testing has also become a marketing tool. The U.K. manufacturer of Marmite recently tried to solve the mystery of why some Brits love the yeast extract spread while others hate it, finding SNPs that predicted whether someone would like it or not. The company is now offering free genetic testing to curious customers as part of a marketing campaign.
California startup Vinome offers customers a curated wine service based on a genetically determined individual taste profile, or as the site calls it, “a little science and a lot of fun.” The site also requires consumers to agree to Vinome keeping their data in their “secure research database for use by Vinome or its research affiliates.”
Taking action
Even if consumers understand their genetic risks, there’s a question of what they can do about them.
Genetic tests for breast and ovarian cancer risk, for example, could prompt women to get mammograms at an earlier age or at a more frequent interval. For high risk women, they could get prophylactic mastectomies or have their ovaries removed. But for conditions like Alzheimer’s or Parkinson’s, there’s not much individuals can do to lower their risks.
The Food and Drug Administration does not allow 23andMe to report genetic tests that can be used as a diagnostic tools, such as the BRCA 1 and 2 breast cancer genes. Customers must decide whether they want their Alzheimer’s or Parkinson’s result, and if so, must read additional information that helps them put their potential risk into context.
23andMe tests for hereditary thrombophilia, a condition that leads to blood clots in blood vessels, often in the legs. It affects only 5 percent of people of Northern European descent, and is much rarer among those with Asian or African roots. Genetic clinics usually test for it in individuals who have had a blood clot or have a family history of the condition.
Those who test positive could wear support hose on long flights or avoid birth control pills that can increase their risk. Otherwise they’re told to live a healthy lifestyle and avoid smoking.
“We encourage all our patients to have healthy lifestyles, physical activity, intellectual activity, reading books, that kind of stuff,” Wiszniewski said. “But we cannot start taking a magic pill that would decrease the risk of those conditions.”
For most health risks identified through genetic testing, the best advice doctors can give to prevent them is to eat a healthy diet, exercise and don’t smoke. And you don’t need genetic testing to know that.
Family genes
Many of those who have been tested are more interested in the genealogy than their health risks. While 23andMe offers both services, other sites offer only information on your genetic roots.
Justin Hodai received an ancestry testing kit for his birthday. His maternal grandfather had been left in a basket on the doorstep of a Catholic church in Brooklyn, New York, as a baby. His family had always suspected he might have been of Jewish descent. Hodai’s maternal grandmother said she was of German descent. But when the tests came back there was no trace of German or Jewish roots.
“There’s a lot of Russian, East European, a lot of the countries that are on the outside of Germany,” Hodai says. “Maybe they could have been Russian or Ukrainian Jews, there’s no way to tell that.”
Hodai’s father had always told him he was 100 percent Japanese, but the test results showed a small percentage of South Asian ancestry. “When I told him there was South Asian in us, he was adamant to say there isn’t any. We’re Japanese and that’s it,” Hodai said. “I was a little taken aback. My entire life, I had never felt this attitude from him.”
Kirkpatrick warns that individuals who are considering genetic testing should think about whether they really want to know the results. “As much as you warn people, they still don’t think it’s going there, it’s going to happen to them,” she says. “No one really truly thinks that they will be that one.”
But the vast majority of individuals who are tested won’t find any major genetic risks in their health profile.
“Most people don’t get a surprise,” she says. “But if we start testing enough things, everybody’s going to find at least one thing. That’s part of being human and having a billion nucleotides. If you just look hard enough, everybody will be just little bit different and maybe in a way that puts them at risk for something.”
That raises concern that genetic testing could prompt people to chase ghosts. Even a minor uptick in risk could lead to a cascade effect, in which people concerned about their genetic reports get more imaging or laboratory tests, leading to more invasive procedures or tests with the potential of treating an anomaly that would never have caused any problems.
Additional imaging tests come with exposure to radiation and carry the risk of finding false positives, all of which would increase health care costs.
Two decades ago, the cost of genetic testing was so high it seemed inconceivable that large numbers of patients could get the testing done. Now, as testing has dropped below $200, many are worried the costs will come not with testing, but in interpreting and following up the massive amount of data in consumers’ hands.
Wasting time
Doctors are used to talking to patients about treatments or services they read about in the media or see in television advertising. But genetic testing has the potential of adding a significant burden to their already limited time with each patient.
“It’s frustrating for genetic counselors or medical geneticists to have people bring in 23andMe raw data and interpretation because we’re missing what’s really important in their family history and spending time on stuff that is of lower meaning,” Pettersen said. “Maybe there’s a very strong family history of lung cancer or something, but they didn’t have any SNPs for lung cancer, so they don’t want to know about that. They want to know about Alzheimer’s disease.”
In the PGen study on how individuals are using genetic test results, 63 percent said they would take their results to their primary care physician. Six months later, 27 percent said they had done so and 8 percent shared with another health care provider. About 10 percent said they had some kind of test, exam or procedure, done as a result of their information.
“Even though that’s a minority, if you think about how many people are doing this, you have a lot of potential downstream effects on their health care,” said Dr. Scott Roberts, director of the Public Health Genetics Program at the University of Michigan. “Unfortunately, our study doesn’t tell us about what ultimately happened.”
The researchers found that people generally didn’t overreact to their genetic test results.
“One of the things they were concerned about was people were going to get a BRCA positive result, and somehow would have prophylactic mastectomy,” Roberts said. “But I think that’s just very unrealistic. That test would automatically be redone in a clinical setting. They wouldn’t just take that at face value.”
The researchers found that patients were unlikely to make changes without first consulting their doctor.
“There was a lot of concerns, too, about the pharmacogenomics information: Are people going to consult their doctors or just start changing medications, and discontinuing them?” Roberts said. “That did seem to be vanishingly rare that anybody reported a medication change, let alone without consulting their doctor.”
Of those patients who learned they would have some atypical reaction to prescription drugs based on their genetic tests, fewer than 6 percent reported changing a medication, and most did so only after consulting with their physician. A small percentage, less than 1 percent, made changes on their own.
In one case, a woman learned she was at increased risk for muscle pain from statins, and reduced the dose of her cholesterol medication as a result. Based on her family history of heart disease, diabetes and cholesterol, the health risk of heart disease likely far outweighed her risk of muscle pain, the researchers said.
Another woman found she was at increased risk for blood clots and consulted her doctor, who lowered her dose of oral contraceptives in response.
“My sense is that, not to say that there aren’t people with misunderstandings, but for the most part, people are getting the key take-home messages, and not taking drastic actions,” Roberts said. “I do think some of the fears seem to be a little bit overblown from my perspective.”
In fact, few people made any changes at all when they learned about their genetic health risks. When researchers surveyed the 12 to 24 percent of individuals who received elevated risk estimates for prostate, breast and colon cancer, they found few had made any changes in their diet, exercise, supplement use, advanced care planning or cancer screening. The one exception was among men at higher risk for prostate cancer, who changed their vitamin or supplement use.
That could be because any sort of behavior change is hard, or it could reflect a sort of fatalistic view of genetics.
“Taking genetic tests can give you a mindset that genes are everything, that everything about us, we can attribute to genes,” said Ricki Lewis, a genetics textbook author from Schenectady, New York. “That’s the opposite of empowering. There are so many things you can change, like intelligence, with environmental input that empowers you to do something.”
The promise of genetic testing is that it can alert people to health risks while there’s still time to prevent them. But there is no study showing that people who get direct-to-consumer genetic tests have better medical outcomes or live longer than those who do not. To establish the usefulness of genetic tests, proponents will have to show that these tests can identify patients at risk before they develop symptoms and that early intervention can improve their outcomes.
Potential gains
Some genetic experts, however, believe the genetic testing revolution has profound benefits for consumers and that 23andMe’s experience with the FDA is keeping valuable information about health risks out of people’s hands.
“I think the FDA has blinded the country from knowing about their health,” said Stuart Kim, a genetics expert and professor emeritus at Stanford University. “They took all this information and said nobody gets to use it, because we’re not sure if it’s being presented in an FDA-approved way.”
Kim has published papers on genetic risks for heart disease, kidney disease and high blood pressure. Some of those studies found a 5 percent change in risk for those conditions with certain variants.
“It’s not a really big change in risk, but who’s to say whether or not it’s useful,” he says. “I think you should have the opportunity to use the data that’s being published. There’s a lot more harm being done, than harm being prevented, by just blinding everyone to all of the information.”
Others have raised privacy concerns about genetic data housed at 23andMe or other genetic websites. Could individuals at high risk for Alzheimer’s or cancer be discriminated against if employers found out? Would insurance companies decline to cover or charge more for individuals based on their genetic risks?
Congress passed the Genetic Information Nondiscrimination Act of 2008, also referred to as GINA, to protect Americans from discrimination based on their DNA, and Kim said concerns are overblown.
“This whole idea that it has to be private, I think, is very strange,” he says. “It reminds me of people not wanting to have their pictures taken because it’s going to steal your soul. I think people are worried about it on some psychological level that doesn’t make any sense.”
23andMe stores the genetic profiles of customers and asks for permission to use the de-identified data for research purposes. The company has more than 1 million customers in its genetic database, and about 80 percent had consented to have their genetic profiles used for research. That’s already started to pay dividends. The database has allowed researchers to find two new genetic variants associated with Parkinson’s disease in less than 18 months.
“I didn’t like 23andme at first, and then I started to realize they were doing a lot of good,” Lewis said. “They were able to find the Parkinson’s gene in months because they had the power of numbers, instead of doing a little NIH study that would take a decade.”
The ability to do genetic testing so quickly and inexpensively has researchers giddy about the potential. Already doctors are starting to use genetics to determine what drugs will be work best in a patient, and how likely they are to cause side effects. Genetic tests are already being used to identify high risk patients for more frequent cancer screening, but could soon be used to fine tune mammography or PSA screening guidelines. Meanwhile, genetic researchers are moving beyond looking at individual SNPs, and looking at genetic profiles that take into account dozens of genetic variants and how they interact to affect health risks.
There is concern that the more personalized medicine becomes, the more expensive it will be, putting it out of reach for anyone beyond the most affluent. But others believe that once the benefits of genetic testing can be proven, and that people can start to prevent diseases before they happen, insurance companies may opt to have everyone’s genome analyzed at birth.
While there are legitimate concerns that consumers may not fully understand the health risks provided by such easy access to genetics testing, it may be too late to debate if they should have it.
“I kind of look at this as this is our reality, and we have to make the best of it,” Kirkpatrick said. People are telling us that they want this information, and we now need to figure out a way to try to get the highest quality information to the greatest number of people,” Kirkpatrick said. “Genetics is complicated. It doesn’t mean that people can’t understand it. They just shouldn’t expect to understand it all at once.” •
“The genes that they’re choosing to test puzzle us: Why these? … If we were designing a clinical test that would be helpful to people for their own health and prevention, we would pick a whole different group of genes to study.”— Barb Pettersen, a genetic counselor in Bend


